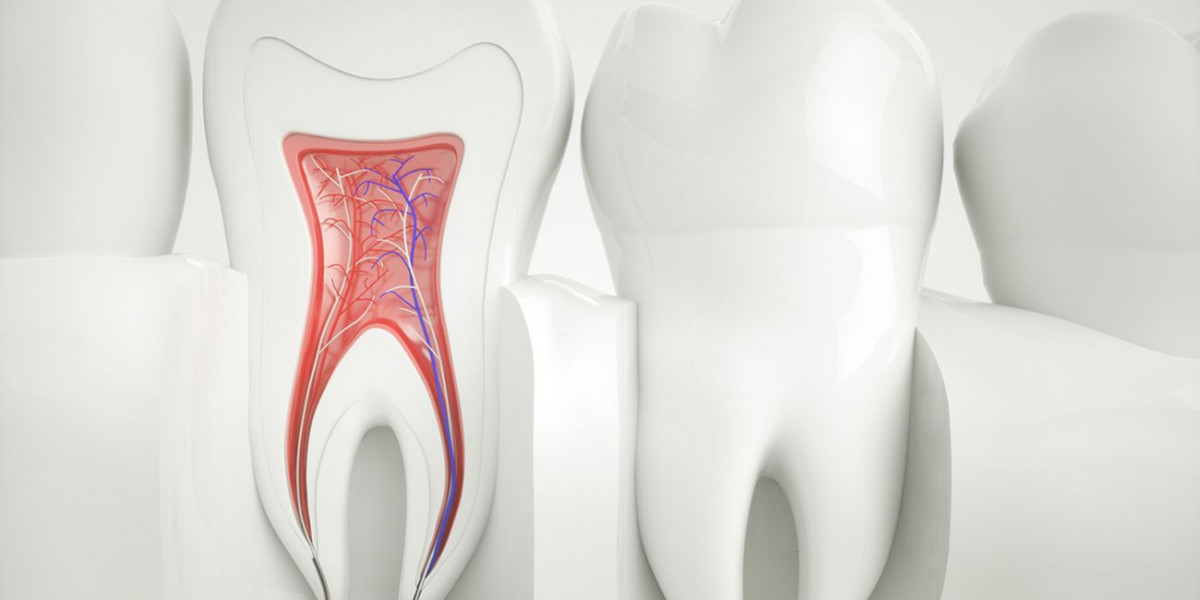
Root canal therapy, also known as endodontic treatment, is a dental procedure aimed at saving a tooth that is severely decayed, infected, or damaged. The procedure involves removing the infected or inflamed pulp from inside the tooth, cleaning and disinfecting the root canals, and sealing the tooth to prevent further infection. While the primary goal of root canal therapy is mechanical removal of infection, antibiotics can sometimes play a supportive role in managing oral infections. Understanding when and how antibiotics are used in root canal therapy is important for patients to make informed decisions about their care. If you are experiencing severe tooth pain, seeking professional Root Canal Treatment in Islamabad can help save your natural tooth and prevent further infection.
When Are Antibiotics Used in Root Canal Therapy?
Antibiotics are not routinely prescribed for every root canal procedure. In most cases, the infection is confined to the pulp of the tooth, and the mechanical cleaning and filling of the canals is sufficient to eliminate bacteria. The body’s immune system, combined with proper dental intervention, usually resolves the infection without the need for systemic antibiotics.
However, antibiotics may be recommended in certain situations, including:
Spread of Infection Beyond the Tooth: If a tooth infection has spread to surrounding tissues, causing facial swelling, cellulitis, or abscess formation, antibiotics may be necessary to prevent further spread of bacteria.
Systemic Symptoms: Patients who experience fever, malaise, or swelling in the lymph nodes due to a dental infection may require antibiotics as part of their treatment plan.
Immune Compromised Patients: Individuals with weakened immune systems—such as those with diabetes, cancer, or autoimmune conditions—may be at higher risk for complications from dental infections. Antibiotics may be used to help prevent severe systemic infection.
Prevention of Infection in High-Risk Cases: Occasionally, antibiotics are prescribed prophylactically for patients with certain heart conditions or joint replacements, in consultation with their physician, to reduce the risk of infective endocarditis or other complications.
How Antibiotics Work in Dental Infections
Antibiotics help the body fight bacterial infections by either killing bacteria (bactericidal) or preventing their growth and replication (bacteriostatic). In dental infections, antibiotics help reduce bacterial load, control the spread of infection, and minimize systemic complications. Commonly used antibiotics in dental practice include amoxicillin, penicillin, and clindamycin, among others. The choice of antibiotic and duration of treatment depends on the severity of the infection, patient health status, and any known allergies.
Why Antibiotics Are Not a Substitute for Root Canal Treatment
It is important to understand that antibiotics alone cannot cure the source of a dental infection within the tooth. Since the pulp tissue inside a tooth is enclosed and often has poor blood supply, systemic antibiotics may not reach all areas of infection effectively. Root canal therapy is required to remove the infected tissue directly and prevent recurrence. Prescribing antibiotics without performing the necessary dental procedure is generally ineffective and may lead to prolonged pain, worsening infection, or complications.
Risks of Unnecessary Antibiotic Use
Overuse or inappropriate use of antibiotics can have significant consequences. Common risks include gastrointestinal disturbances, allergic reactions, and the development of antibiotic-resistant bacteria. Misuse of antibiotics can make future infections harder to treat and contribute to broader public health challenges. Dentists carefully weigh the benefits and risks before prescribing antibiotics to ensure they are used only when medically necessary.
Post-Procedure Considerations
When antibiotics are prescribed in conjunction with root canal therapy, patients must complete the full course as directed, even if symptoms improve before the medication is finished. Stopping antibiotics early can allow bacteria to survive and lead to recurrent infection. Additionally, patients should continue following post-procedure care instructions, including maintaining oral hygiene, avoiding hard foods, and attending follow-up dental visits to ensure proper healing and restoration of the treated tooth.
Conclusion
Antibiotics play a supportive, but limited, role in root canal therapy. Their primary purpose is to control the spread of infection and manage systemic symptoms, particularly in cases where the infection extends beyond the tooth or in patients with compromised immune systems. They are not a replacement for the mechanical removal of infected pulp, which is the core of root canal therapy. Careful and judicious use of antibiotics helps maximize patient safety, minimize complications, and promote effective healing.